10th Edition of International Conference on
Antimicrobial Resistance
Throughout history, humans have combated bacterial and other microorganisms using traditional medicine and natural remedies. As modern biomedical approaches to diseases and other ailments have become the norm, traditional medicine has remained an important part of medical and public health care. However, the growing resistance of pathogenic microorganisms to available therapeutic agents poses an ethical and clinical challenge that can only be responsibly tackled by a combination of modern and traditional strategies. Traditional medicinal plants and their compounds have been used to treat infections since the dawn of humanity as antibiotics were not available until earlier into the twentieth century. Their active ingredients have mostly antibiotic-like properties and have been proven to have a wide range of biological effects against a variety of pathogens. Unfortunately, bacteria and other microorganisms can become resistant to these treatments, as well as to more contemporary antibioticsv. The development of resistance to traditional medicines is a concern, but it is not necessarily a new phenomenon since there is evidence of fungal and bacterial resistance to conventional drugs from over 1,000 years ago. Furthermore, various traditional medicines have been used for millennia to treat antibiotic-resistant infections, a prime example being streptomycin-resistant tuberculosis that polyherbal medicines were used to treat in India since the 1960’s. In response to this troubling development, strategies to minimize the emergence of antimicrobial resistance (AMR) and sustain the efficacy of traditional medicines are needed. The World Health Organization (WHO) outlines best practices for the management of AMR including the safe and judicious use of traditional medicines and prevention of the spread of resistance. These strategies involve better surveillance and reporting of AMR, development of evidence-based rational therapeutic guidelines, research into new active ingredients, and the promotion of practices within traditional medicine that limit the emergence, spread, and transmission of resistant microbes. In conclusion, traditional medicine has been a crucial part of medical history and still remains an important part of public health care today, but AMR has become a serious challenge that needs to be taken into consideration. To ensure the safety and efficacy of traditional medicines, the WHO’s best practices for the management of AMR need to be adopted both globally and locally. In addition, further research into the active ingredients present in traditional medicines is required in order to discover and isolate new compounds that can be used to combat resistant pathogens.
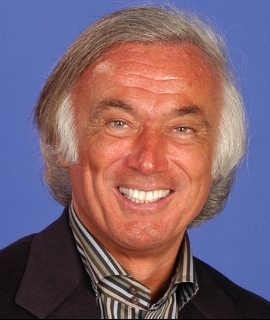
Kenneth R Pelletier
University of California School of Medicine, United States
Marilyn Allen
American Acupuncture Council, United States


